Bladder irrigation and bladder washout are two related but distinct procedures used to manage urinary tract issues by flushing the bladder with sterile fluid. Bladder irrigation generally refers to the continuous or intermittent instillation of irrigating solution—most commonly sterile saline—through a urinary catheter to prevent catheter blockage, dilute hematuria, or deliver medications. It is often employed in postoperative care after urologic surgery, during episodes of gross hematuria, or when debris and sediment threaten catheter patency. By maintaining a clear drainage pathway, irrigation helps reduce the risk of bladder spasms, infection, and clot retention.
Bladder washout, on the other hand, is typically a one-time or short-duration manual flushing procedure aimed at removing encrustations, mucus, blood clots, or crystalline deposits that have accumulated around and within an indwelling catheter. Unlike routine irrigation, which may be scheduled at set intervals, washout is performed in response to catheter dysfunction—such as reduced urine flow or visible sediment in the drainage bag. The technique usually involves instilling a measured volume of solution, allowing it to dwell briefly, and then aspirating it back to extract particulate matter.
Although both procedures share the common goal of maintaining catheter function and bladder health, they differ in timing, purpose, and technique. Bladder irrigation is more preventive or therapeutic in ongoing care, whereas bladder washout is reactive, targeting existing obstructions. Proper selection between irrigation and washout depends on patient factors—such as bleeding risk, infection status, and catheter type—as well as clinical objectives. Below is a comparative overview:
| Feature | Bladder Irrigation | Bladder Washout |
|---|---|---|
| Definition | Continuous or intermittent flushing to maintain patency | Manual, targeted flushing to remove existing debris |
| Primary Purpose | Prevent blockage, dilute hematuria, deliver meds | Clear encrustations, blood clots, mucus from catheter |
| Typical Indications | Post-urologic surgery, gross hematuria, long-term cath | Catheter blockage, reduced flow, visible sediment |
| Technique | Gravity-drip or syringe instillation, continuous or timed | Inject-dwell-aspirate cycle with syringe |
| Solutions Used | Sterile saline ± anticoagulant/antibiotic additives | Sterile saline; occasionally enzymatic or acidic agents |
| Frequency | Scheduled (e.g., every 4–6 hours) or continuous | As needed when obstruction is identified |
| Advantages | Prevents complications proactively; can deliver drugs | Directly removes blockages; rapid flow restoration |
| Risks & Considerations | Infection risk, fluid overload, electrolyte shifts | Urothelial irritation, incomplete debris removal |
Careful adherence to aseptic technique, accurate solution selection, and monitoring for signs of infection or fluid imbalance are vital to ensure both bladder irrigation and washout achieve their intended benefits without causing additional harm.
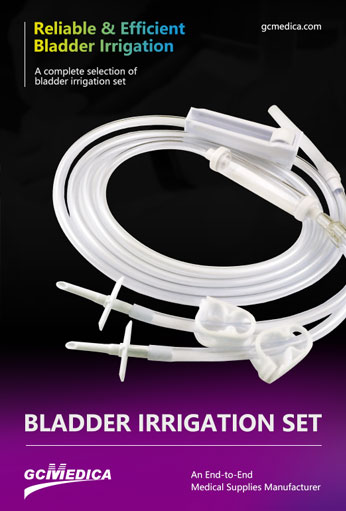
| Bladder Irrigation Set > |


 Français
Français Español
Español Products
Products

 About Us
About Us