A chest tube drainage system (CDS) is a sterile, closed apparatus designed to remove air, blood, or other fluids from the pleural space to facilitate lung re‑expansion and restore normal intrathoracic pressure. It employs a one‑way underwater seal or mechanical valve to prevent retrograde air or fluid entry, ensuring unidirectional flow out of the pleural cavity. Modern systems range from traditional three‑chamber “wet” units to advanced digital dry systems offering precise suction regulation and real‑time leak monitoring.
Chest Tube Drainage System (CDS) >
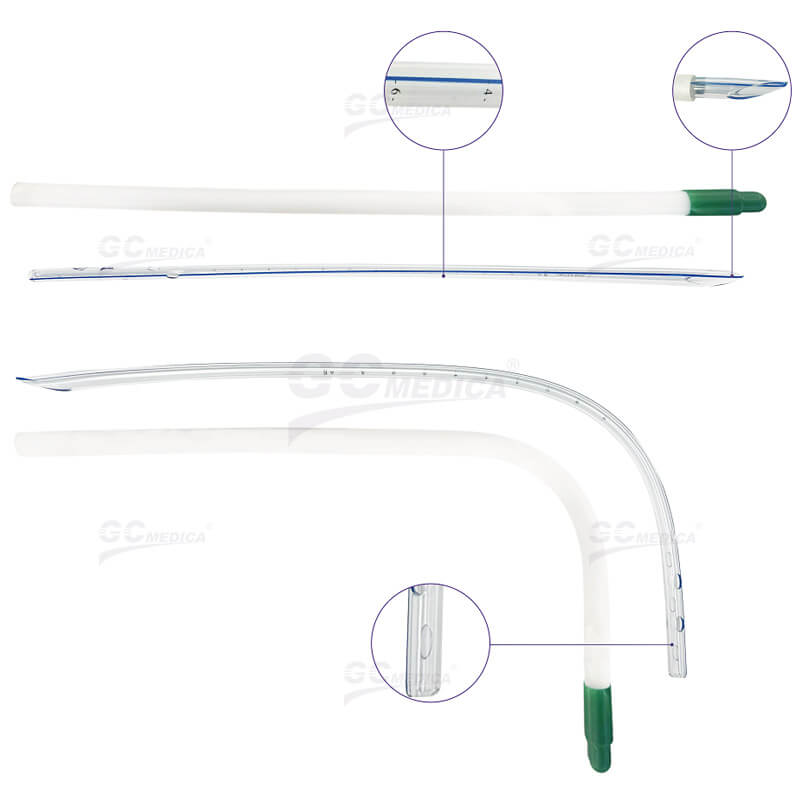
Components
Traditional CDS units feature three primary chambers: a collection chamber for effluent, a water‑seal chamber acting as a one‑way valve, and a suction‑control chamber for regulating negative pressure. The collection chamber allows visualization and measurement of drainage output, aiding in clinical assessment of hemorrhage or fluid overload. The water‑seal chamber typically contains sterile water to maintain a seal, where intermittent bubbling indicates air evacuation and continuous bubbling may signal an ongoing air leak. The suction‑control chamber adjusts negative pressure, commonly set between –10 to –20 cm H₂O, by varying the water column height or via dry regulators in “wet‑dry” systems.
Types and Mechanism
In “wet” systems, suction is regulated through a water column whose depth determines the applied negative pressure, independent of wall suction variability. “Dry” and “wet‑dry” systems replace the water column with mechanical regulators, eliminating risks of spillage and facilitating portability. Digital systems incorporate electronic sensors, providing continuous readouts of intrapleural pressure, quantitative leak detection, and data storage for trend analysis. Flutter‑valve devices such as Heimlich valves offer a lightweight alternative for ambulatory patients with pneumothorax, allowing mobility without bulky canisters.
Clinical Considerations
Indications for CDS include traumatic or spontaneous pneumothorax, postoperative thoracic surgery care, hemothorax, empyema, and large pleural effusions from malignancy or heart failure. Proper device setup mandates ensuring all connections are airtight, priming water levels per manufacturer guidelines and positioning the system below chest level for gravity‑assisted drainage. Regular monitoring includes hourly assessment of fluid character and volume, inspection of water‑seal fluctuations, and evaluation of insertion‑site integrity for infection or subcutaneous emphysema. When drainage decreases below clinician‑defined thresholds (often < 200 mL/24 h) and imaging confirms lung re‑expansion, brief clamping trials may precede safe tube removal. Adherence to CDS protocols minimizes complications such as tube dislodgement, blockage, or persistent air leaks, thereby optimizing patient recovery and reducing hospital stay duration.
Related Products


 Français
Français Español
Español Products
Products

 About Us
About Us