Tracheostomy tubes are essential airway devices used to secure ventilation in pediatric patients who require long-term respiratory support, airway protection, or relief from upper airway obstruction. Selecting the correct tube size is crucial: an undersized tube can increase airway resistance and impede effective ventilation, while an oversized tube may traumatize the delicate tracheal mucosa or interfere with normal airway clearance. Pediatric tracheostomy tube sizes are typically categorized by internal diameter (ID), outer diameter (OD), length, and whether they are cuffed or uncuffed. Below is an overview of commonly used sizes across different pediatric age groups.
| Age Group | Tube Type | Internal Diameter (ID, mm) | Outer Diameter (OD, mm) | Length (cm) | Cuffed? |
|---|---|---|---|---|---|
| Neonate (0–1 mo) | Standard | 2.5 | 4.3 | 3.5 | Uncuffed |
| Infant (1–12 mo) | Standard | 3.0 | 5.0 | 4.0 | Uncuffed |
| Toddler (1–3 yr) | Standard | 3.5 | 5.7 | 4.5 | Uncuffed |
| Preschool (3–6 yr) | Standard | 4.0 | 6.4 | 5.0 | Uncuffed/Cuffed |
| School‑Age (6–12 yr) | Standard | 4.5 | 7.1 | 5.5 | Cuffed |
| Adolescent (>12 yr) | Standard | 5.0–6.0 | 7.8–8.5 | 6.0–6.5 | Cuffed |
When choosing a tube, clinicians must consider not only the patient’s chronological age but also weight, neck length, and underlying airway anatomy. Uncuffed tubes are generally preferred for infants and young children to minimize tracheal injury, whereas cuffed tubes may be indicated in older children when positive-pressure ventilation is required or to reduce aspiration risk. Length selection ensures that the distal tip lies approximately 1.5–2 cm above the carina, avoiding endobronchial migration or excessive proximity to the larynx.
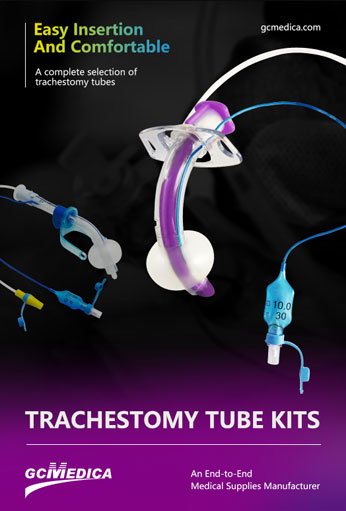
Beyond mere dimensional fit, the material and design of the tube contribute to patient comfort and safety. Most pediatric tracheostomy tubes are made of medical‑grade PVC or silicone, which balance flexibility with sufficient rigidity to maintain patency. Some tubes feature inner cannulas that can be removed for cleaning or replaced in case of obstruction, reducing the need for repeated tube changes. Fenestrated designs allow for speech development in older children but must be used cautiously to avoid granulation tissue formation.
Regular assessment and tube exchanges are part of ongoing tracheostomy care. As the child grows, tube upsizing is often required every 6–12 months under controlled settings. Continuous monitoring for complications—such as tube blockage, mucosal ulceration, infection, or accidental decannulation—is vital. Correct tube sizing, combined with diligent stoma and tube maintenance, underpins successful long‑term tracheostomy management in the pediatric population.
| Tracheostomy Tubes > |


 Français
Français Español
Español Products
Products

 About Us
About Us